How To Desensitize The Tip Domain_10
Introduction
Not-steroidal anti-inflammatory drugs (NSAIDs) and aspirin are amidst the nigh normally prescribed and used drugs in the globe and, along with antibiotics, are the top two (depending on the population studied) causes of adverse drug reactions [1]. It is estimated that hypersensitivity to NSAIDs affects from 0.v to 1.9 % of full general population [2], but in sure populations similar patients with bronchial asthma or with chronic rhinosinusitis, the prevalence of NSAIDs hypersensitivity is much college [3, four••].
The management of drug hypersensitivity reactions e'er starts with advice on abstention of the culprit drug and whatever cross-reactive compounds [5••], but in some patients, consecration of tolerance to the drug can exist also considered. In case of NSAIDs hypersensitivity, despite big number of compounds belonging to this group, simply desensitization to aspirin has been sufficiently documented.
When to desensitize a patient with NSAIDs hypersensitivity?
While considering aspirin desensitization in a patient with a history of hypersensitivity to NSAIDs, the following aspects have to be taken into consideration:
- ane.
Determination of a subtype of NSAIDs hypersensitivity, since desensitization is possible only for some subtypes, while in other subtypes desensitization may be contraindicated.
- 2.
Analysis of clinical do good from handling with aspirin (NSAID) afterward desensitization.
- 3.
General safety of desensitization procedure.
- 4.
Option of desensitization protocol—different protocols are used depending on the indication for desensitization.
Subtypes of NSAIDs hypersensitivity and possibility of desensitization
NSAIDs tin can evoke a wide spectrum of adverse drug reactions (respiratory, cutaneous, anaphylactic, or other organ-specific) involving different pathomechanisms. Consecration of tolerance to aspirin is possible and indicated simply in two subtypes of NSAIDs hypersensitivity: (ane) NSAIDs-exacerbated respiratory disease (NERD) and (ii) NSAIDs-induced urticaria/angioedema (NIUA), thus determination of the blazon of hypersensitivity is prerequisite to successful desensitization.
According to novel nomenclature of NSAIDs hypersensitivity, either immunologically and non-immunologically mediated reactions can be distinguished [four••] (Table 1). Most of the hypersensitivity reactions to NSAIDs are non-immunologically mediated but are cross-reactive hypersensitivity reactions every bit the patients usually practise not tolerate all NSAIDs with COX-i inhibitory activeness. Among these cantankerous-reactive reactions, 3 clinical subtypes tin be distinguished:
NSAIDs-exacerbated respiratory disease (NERD)
This hypersensitivity reaction is manifested mainly by respiratory symptoms and occurs in patients with underlying chronic airway disease like asthma and/or rhinosinusitis with nasal polyps. NSAIDs-induced bronchial symptoms (dyspnea, cough) ordinarily announced within ane–2 h and are preceded past nasal symptoms (rhinorrhea, nasal congestion) [iv••]. Other extrabronchial symptoms: ocular, cutaneous (flushing of the upper thorax, urticaria, and/or angioedema) or gastric are less frequent [6]. Typical natural history of the diseases starts with evolution of chronic rhinosinusitis with polyps, followed by asthma, which usually precede the kickoff of hypersensitivity reaction [3]. Patients with NERD commonly have more astringent asthma as compared to aspirin-tolerant asthmatics [vii]. Furthermore, chronic rhinosinusitis in NERD patients is usually more than severe, very often complicated by recurrent nasal polyp formation which responds less to surgical treatment [3]. NERD is i of non-immunological, cross-reactive types of hypersensitivity every bit patients hypersensitive to 1 NSAIDs react to aspirin and other NSAIDs which are COX-1 inhibitors, while weak COX-i inhibitors or preferential COX-2 inhibitors are ordinarily well tolerated [eight–ten].
Aspirin desensitization
Aspirin desensitization in this subtype of hypersensitivity can be easily accomplished, and treatment with aspirin after desensitization may exist benign for improving symptoms of the underlying chronic diseases, asthma, and rhinosinusitis with nasal polyps [11••, 12].
NSAIDs-exacerbated cutaneous disease (NECD)
This type of hypersensitivity is observed in patients suffering from chronic spontaneous urticaria. Clinical symptoms (urticaria and angioedema) typically occur 0.five to half-dozen h after ingestion of NSAIDs. NSAIDs-induced reactions are less frequent and less intense when chronic urticaria is in remission or under command. The mechanism of the reaction, similarly to NERD, is related to the inhibition of cyclooxygenase −1 by a culprit drug, resulting in increased generation of cysteinyl leukotrienes [13]. Thus, patients with NECD would have a cantankerous-reaction with COX-1 inhibitors, while selective COX-2 inhibitors are generally well tolerated by the majority of them [14].
Aspirin desensitization
In this subtype of NSAIDs hypersensitivity, the tolerance of aspirin may be difficult to achieve and in some patients, cutaneous symptoms may be even exacerbated by the procedure [15]. Thus, aspirin desensitization in NECD patients is not recommended, even though at that place have been some reports of successful induction of tolerance to aspirin [16, 17].
NSAIDs-induced urticaria/angioedema (NIUA)
The clinical pattern of NSAID-induced symptoms is similar to NECD (wheals and/or angioedema); notwithstanding, in dissimilarity to NECD, patients with NIUA do not accept history of chronic spontaneous urticaria. The mechanism is thought to be related to COX-1 inhibition, but it has non been well documented [14, xviii•].
Aspirin desensitization
Aspirin desensitization is possible in most patients. Tolerance state tin exist easily maintained with continuous intake of aspirin [nineteen••, 20, 21].
The ii remaining subtypes of NSAIDs hypersensitivity are immunologically mediated and are distinguished past intolerance of a single drug (chemic molecule) and proficient tolerance of other chemically unrelated NSAIDs.
Unmarried NSAIDs-induced urticaria/angioedema/anaphylaxis (SNIUAA)
A subpopulation of patients reports firsthand hypersensitivity reaction to a single NSAID (or to several NSAIDs but belonging to the aforementioned chemical grouping). Patients usually nowadays with a history of expert tolerance to other chemically unrelated NSAIDs, including aspirin [18•]. The symptoms range from mild urticaria and localized angioedema to laryngeal edema and anaphylaxis and usually develop within first 60 minutes after the drug intake [eighteen•]. However, in some instances, symptoms may develop inside minutes or fifty-fifty seconds (e.g., after intravenous injection of metamizole) [22]. These subjects are normally otherwise healthy individuals without any specific underlying chronic disease. The reactions are most often induced by pyrazolones, ibuprofen, or diclofenac; nevertheless, other NSAIDs as paracetamol have been implicated equally well. Aspirin incidentally evokes hypersensitivity reactions in this machinery.
Aspirin desensitization
At that place is no information on desensitization in this type of reactions. As symptoms of hypersensitivity are unremarkably evoked past a single drug, the chemical compound with different chemic construction can be prescribed and volition exist well tolerated.
NSAIDs-induced delayed hypersensitivity reactions (NIDHR)
Reactions developing usually subsequently more than than 24 h afterward the drug intake are considered to represent delayed blazon of immunological hypersensitivity. Delayed cutaneous manifestation are the most mutual and involve maculopapular eruptions (MPE), fixed drug eruptions (FDE), photosensitivity reactions, delayed urticaria [23–25], and contact dermatitis [26]. In improver, severe drug hypersensitivity reactions (drug induced hypersensitivity syndrome (DIHS), acute generalized exanthematous pustulosis (AGEP), and severe cutaneous adverse reactions (SCAR) [27–29] as well every bit organ-specific injury (pneumonitis and nephritis) may occur [thirty].
The presumed immunological mechanism involves the stimulation of drug-specific CD4+ and CD8+ T cells through their T jail cell receptors (TCR) and represents a delayed type hypersensitivity (blazon IV according to Gell Coombs) T cell-dependent mechanisms have been documented in delayed urticaria, MPE induced past aceclophenac [31] and metamizol and in SCAR induced by ibuprofen [32, 33].
Aspirin desensitization
In that location is no data on desensitization to aspirin. In nigh patients with delayed type hypersensitivity reactions (SCAR, Clothes, AGEP, and pneumonitis and nephritis), a claiming with culprit drug is generally contraindicated [five••, 34]. In instance of less severe delayed drug reactions, due east.g., maculopapular eruptions, there is no attempts of desensitization have been reported. Furthermore, since the reactions are evoked past a unmarried NSAID, the culprit drug tin can exist usually replaced.
Clinical indications to NSAIDs desensitization
Avoidance of culprit drug likewise as other cross-reactive compounds is the first recommendation in the management of NSAIDs hypersensitivity [4••]. If the handling with analgesic/anti-inflammatory drug is needed, a non-cross-reactive drug should be given, selected depending on the known mechanism. Most patients with cross-reactive, not-immunologically mediated types of NSAIDs hypersensitivity will tolerate preferential COX-2 inhibitors similar meloxicam or nimesulide or selective COX-two inhibitors (celecoxib) with relevant anti-inflammatory effect. Aspirin, however, take additional important pharmacological furnishings going across anti-inflammatory or analgesic activity. As a cardinal anti-platelet drug, aspirin is recommended for primary and secondary prevention in patients with a loftier take chances of major cardiovascular events (expiry, myocardial infarction, or stroke) [35, 36]. Contempo information evidence that low doses of aspirin can decrease the hazard of certain malignant tumors development: e.grand., colorectal cancer [37] or ovarian cancer [38].
Moreover, in patients with NSAIDs-exacerbated respiratory disease daily treatment with aspirin tin bring additional benign effects similar alleviation of nasal symptoms, decreased formation of nasal polyps, and reduced need for oral corticosteroids and sinus surgeries. Clinical indications for aspirin desensitization are listed in Table two.
Aspirin desensitization in patients with demand for anti-platelet handling
Cardiovascular events are the major crusade of mortality in developed countries [39]. Aspirin is the most studied anti-platelet amanuensis in this context of prevention and treatment of cardiovascular disease (coronary avenue disease, stroke, peripheral avenue disease). Aspirin decreases mortality and reinfarction when given as short-term therapy for acute myocardial infarction [forty], when given to patients with unstable angina [41], and when given every bit long-term secondary preventive therapy in wide range of patients with cardiovascular disease [42].
Although, in contempo years, novel anti-platelet drugs become available like adenosine diphosphate receptor inhibitors (clopidogrel, prasugrel, ticlopidine, ticagrelor), glycoprotein IIb/IIIa inhibitors (abciximab, eptifibatide), or adenosine reuptake inhibitors (dypirimidamole). Given its relative safety and low price, aspirin will continue to be an important agent in the handling and prevention of cardiovascular diseases.
Moreover, in certain clinical situations, dual anti-platelet therapy is mandatory, e.chiliad., afterward myocardial infarction and/or afterwards stent implantation [43, 44]. A great majority of patients subsequently cardiovascular events will crave handling with aspirin till the end of life [43].
For patient with aspirin hypersensitivity and acute coronary syndrome, either use of clopidogrel or aspirin desensitization is recommended by cardiologists (ACC/AHA guidelines from 2007 [45] and ESC guidelines [46]).
Although there is plenty of data on safety of aspirin desensitization in patients with stable coronary heart affliction, much more challenging is taking decision on aspirin desensitization in patient with acute coronary syndrome equally patient very ofttimes received drugs that are contraindicated during desensitization (beta blockers and ACE inhibitors) and there is fear that hypersensitivity reaction which may occur can further destabilize the patient. Moreover, desensitization tin can exist avoided past using more than aggressive anti-platelet treatment with intravenous drugs such as abciximab, integrilin, or tirofiban.
There is limited data on aspirin desensitization in acute phase of acute coronary syndrome [47]. De Luca et al. presented in prospective way group of patient undergoing coronary angioplasty (53 % due to acute coronary syndrome) who were desensitized with aspirin. Procedure of intravenous desensitization was constructive in 97.6 % of patients [47]. Thus, it seems that at least some of the proposed protocols can be implemented safely even in patients with acute coronary syndrome. However, equally the hypersensitivity reaction was not proven by challenge test, it is not clear how many of those patients were really hypersensitive. The aspirin desensitization in patients with ACS should be performed afterward stabilization of acute phase, and information technology should be performed in monitored atmospheric condition and past experienced staff.
An interesting approach to ASA-desensitization in patients with coronary avenue illness has been proposed past Cortellini et al. A patient with stable coronary artery disease and history of mild symptoms later NSAIDs intake at start should be challenged with aspirin to confirm hypersensitivity [19]. If a patient presented history of astringent symptoms after NSAID intake, desensitization procedure was done without attempts to confirm hypersensitivity. Interestingly, 29 from 30 patients with history of mild symptoms of urticaria and/or angioedema fully tolerated the cumulative dose of 160 mg of acetylsalicylic acrid during the challenge. There are at least two explanation of this observation, either patients were not hypersensitive or the threshold dose of aspirin to evoke clinical symptoms was not reached during the tolerance test.
Aspirin desensitization and aspirin treatment in patients with NERD
Information technology has been documented that in a subgroup of patients with NSAIDs-exacerbated respiratory disease (NERD), ingestion of aspirin after desensitization results in alleviation of both upper and lower airway symptoms [11••, 12, 48–53]. The long-term effects of aspirin treatment include improvement in nasal symptoms, subtract in the maintenance dose of intranasal glucocorticosteroids, and a subtract in the number of polypectomies [12, fifty, 52, 54]. Aspirin desensitization tin can slow downward regrowth of nasal polyps and prevent further nasal surgeries [55]. Usually, information technology is recommended that aspirin desensitization should follow sinus surgery [55].
Aspirin handling afterwards desensitization may also have an impact on asthma command. When the patients were treated with aspirin for 6 months to 6 years, a significant reduction in hospitalization, emergency room visits, outpatient visits was observed and in some patients, a reduction in daily oral prednisone doses was achieved [12, 49, 50]
There are two placebo-controlled studies that support these benefits. Swierczynska-Kempa et al. [11••] randomly selected both aspirin hypersensitive and aspirin-tolerant asthmatics to aspirin or placebo treatment group. The comeback in nasal symptoms score and reduction in sneezing and nasal blockade was observed just in patients with aspirin hypersensitivity treated with aspirin. The nasal symptoms improved within the first month of handling, and improvement was seen throughout the entire observation period. Still, it has to be noted that computed tomography (CT) sinus scan scores did non change in parallel to clinical improvement. Asthma control was improved, and the dose of inhaled corticosteroids was decreased; however, asthma symptoms score and spirometric values did not alter significantly [11••].
Efficacy of treatment with diverse doses of aspirin from 100 to 1300 mg accept been reported. While some studies study that aspirin dose equally low as 100 mg daily for 1–three years may provide benefit with respect to the recurrence charge per unit of nasal polyps, severity of bronchial asthma and sense of smell in desensitized patients with NERD [51], another studies suggest that clinical efficacy starts from 300 mg/twenty-four hour period [52]. However, information technology seems that the dose should be tailored to the patient and both clinical efficacy and side furnishings should exist taken into consideration while determining the maintenance dose. A study comparison 325 with 650 mg twice a day showed that in almost half of patients, half of the dose was enough while the residual of the patients required higher doses [56]. The reports from Scripps Clinic propose starting with 650 mg twice a day and titrate the dose downward by 325 mg each month, as tolerated [57]. In our dispensary, we desensitize patient to 650 mg of aspirin and requite a maintenance dose of 325 mg twice a day.
In gild to maintain tolerance state, aspirin has to be given on a regular basis—if non, the tolerance country disappears after 2–v days. In most of the studies, aspirin was given in one case or twice a day.
How and where to desensitize?
Aspirin desensitization is a high-risk procedure, which has to be done after assessment of risk-benefit ratio following discussion with a patient. Earlier desensitization, the patient should exist provided with data about procedure risk and benefits and sign the consent.
Desensitization is contraindicated in patients with previous severe, life-threatening cutaneous reactions like Stevens-Johnson syndrome/toxic epidermal necrolysis, DIHS/Wearing apparel, AGEP, erythema multiforme and serum sickness illness, and organ interest [5••, 34]. Take a chance factors for astringent bronchial reaction in patients with NERD during desensitization include severe reaction with autumn of FEV1 > 20 %, uncontrolled asthma, baseline FEV1 less than eighty %, lack of leukotriene modifier premedication, previous emergency section visits due to asthma exacerbation [58].
Where
Desensitization procedure can be performed both in hospital and outpatient setting after run a risk stratification. The severity and fourth dimension class of initial hypersensitivity reaction have to be assessed, and the concomitant use of medication such as beta blockers and ACE inhibitors and the severity of underlying affliction demand to exist taken into consideration [59].
Patients with severe asthma, astute coronary syndrome, patients using beta blockers, angiotensin converting enzyme (ACE) inhibitors, severe life-threatening aspirin hypersensitivity reaction, underlying medical condition that brand direction of hypersensitivity reaction more difficult (eastward.grand., cardiac insufficiency) should be exceptionally desensitized (after careful assessment of risk-benefit ration), only in hospital settings.
If aspirin desensitization is to be performed in the outpatient setting, the following conditions should be fulfilled [59]:
-
A physician experienced in assessing and treating acute, astringent hypersensitivity reactions is immediately available for patient evaluation and treatment.
-
Medically qualified personnel experienced with assessing and treating of severe asthma exacerbation is available to monitor patient.
-
At to the lowest degree 1 feel medical staff member is solely defended to evaluation of patient beingness desensitized until desensitization is completed.
-
The equipment for continuous respiratory and cardiovascular monitoring, spirometry, cardiopulmonary resuscitation, pulsoximetry, is readily available.
In summary, desensitization procedure should exist performed by well-trained, experienced allergists and nurses who are familiar with treatment of acute hypersensitivity reactions and anaphylaxis. Emergency equipment for continuous pulmonary and cardiovascular monitoring and treatment like epinephrine, oxygen, beta-two mimetics, intravenous glucocorticosteroids, antihistamines, glucagon should be available at bedside.
Preparation to desensitization and pretreatment
Patient planned for desensitization should have stable underlying affliction, e.g., asthma. Treatment of chronic diseases should be continued, just drug which can interfere treatment of hypersensitivity reaction like beta blockers or ACE inhibitors should be discontinued/replaced past drugs from other pharmacological groups whenever possible. The Macy's recommendation is to cease antihistamines 48 h before desensitization non to mask naso-ocular symptoms which normally precedes onset of bronchial symptoms and decreasing of FEV1. The use of asthma controller medication prior to desensitization is recommended as they foreclose astringent decreases of FEV1 [60]. Duration of the supervision depends on initial hypersensitivity reaction.
Pretreatment with leukotriene blockers may alleviate symptoms of quantum reaction in patients with NERD by shifting reaction from bronchial to naso-ocular symptoms [threescore].
Desensitization procedures
In most protocols for aspirin desensitization, the procedure begins with provoking the reaction with a standard, as depression every bit possible aspirin dose (threshold dose) followed by administration of increasing doses which usually are well tolerated. Even so, it has been documented that the tolerance country to full dose of aspirin (e.g., 600 mg) can be as well induced, without evoking the initial reaction, past timely and gradual administration of pocket-sized, subthreshold doses of aspirin [61]. Such procedure has been recently referred to every bit "silent desensitization" [62].
At that place are two major types of protocol used in clinical practice for aspirin desensitization depending on the indications for the process: "ho-hum desensitization" protocols used to desensitize patients with NSAIDs-exacerbated respiratory disease and "rapid desensitization" protocols used to desensitize patients with cardiologic indications to use depression doses of aspirin (Table iii)
Protocols for patients with NERD
Several protocols for desensitization of patients with NERD accept been proposed and used [58, 59, 63–67]. The recommended starting dose is between 10 and 30 mg [58, 59, 63, 65], but the time interval betwixt consecutive increasing doses varies from 30 min to 24 h in different protocols [68]. The well-nigh widely used protocols have been proposed past the Scripps Dispensary [63]. One of the proposed schedules advices giving following doses of aspirin: 30, 45, sixty, 100, 150, 325, and 650 mg. The recommended time interval between doses is 3 h, but FEV1 and clinical assessment should be performed every hour or upon presentation of any symptoms. Reaction will likely occur with doses between 20 and 101 mg, and reaction should exist treated immediately.
Following the dose that evoked symptoms (chosen the provoking/threshold dose) and before the next dose of aspirin is given, the patient should completely stabilize, and the respiratory office should return to baseline values. The provoking/threshold dose is normally repeated on the same mean solar day, although some recommend the adjacent morning. If the dose is tolerated, the dose is increased every 3 h (101.25, 162, 325, and 650 mg). The run a risk of a reaction to the repeated threshold dose is small, but if it occurs, the dose should exist repeated again until reactions end and then the side by side highest dose of aspirin may exist given.
Condom of long-term handling with NSAIDs
The incidence of side effects of aspirin treatment in patients with NERD followed by aspirin desensitization varies from 6–32 %. The near common adverse reactions in patients on maintenance therapy are the following:
- 1)
Dyspepsia
- 2)
Haemorrhage from gastrointestinal system
- iii)
Urticaria/angioedema
- iv)
Loss of tolerance and asthma/rhinosinusitis exacerbation
The concomitant apply of proton pump inhibitors can prevent symptoms of dyspepsia, gastric ulceration, and bleeding, but information technology won't preclude bleeding from lower parts of gastrointestinal system. Recently published data indicates that proton pump inhibitors (PPIs) can even exacerbate NSAID-induced intestinal damage at to the lowest degree in part because of significant shifts in enteric microbial populations [69, 70]. Helicobacter pylori, an independent gamble cistron for ulcers, should exist sought out and eradicated in patients at increased gastrointestinal risk, typically those with an ulcer history prior to aspirin desensitization [71].
Protocols for patients with need of anti-platelet treatment
Desensitization protocols for patients who need handling with anti-platelet doses of aspirin differs from protocols used in NERD desensitization because: (a) patients need to be desensitized to lower dose of aspirin—75–150 mg, (b) patients represent unlike subtypes of hypersensitivity (NERD or NIUA), (c) very often, patients require rapid desensitization (patient with acute coronary syndrome).
Several protocols of rapid aspirin desensitization have been published [xix••, 20, 21, 47, 72–77]. These protocols differ in starting dose, time interval betwixt subsequent doses, and number of steps. Rapid protocols usually commencement with lower aspirin dose (from 0.i to 5 mg of ASA) [20, 21, 72, 73], and increasing doses of aspirin are given every 10–xxx min. Protocols consist of five–12 steps. (Table 3)
Interesting, alternative approach to aspirin desensitization was proposed past DeLuca et al. [47] who employed intravenous protocol in patients with myocardial infarction. The desensitization procedure involved intravenous administration of 9 sequential doses of aspirin (ane, 2, 4, eight, xvi, 32, 64, 128, 250 mg) over 4.v h [47]. The protocol appeared to be condom and effective (the success rate reached 97.half dozen %).
At that place is withal lack of consensus, which protocol should exist used for desensitization of cardiac patients, and what are the indication and contraindications to desensitization procedure. Although various authors written report on excellent safety and efficacy of desensitization procedure (from 81–97 % success rate), the existent effectiveness of desensitization is not clear. The assessment of reported furnishings is difficult since well-nigh studies included patients with various, not well divers types of NSAIDs hypersensitivity, diagnosis of hypersensitivity to NSAIDs was based only on clinical history and usually was not confirmed past claiming test.
There is also a fence almost individual aspirin thresholds of aspirin since, as it is known from challenge studies, that some hypersensitive patients may tolerate aspirin in the dose up to 150 mg or even 325 mg. In these patients, anti-platelet treatment with low dose of aspirin after standard "desensitization" procedure can be still below the threshold dose that can evoke reaction [54, 66, 68]. These considerations back up the recommendations that the first step in management of a patient with hypersensitivity reaction to NSAIDs is to confirm the presence of hypersensitivity past a challenge test. Cortellini et al. [19••] documented that more than 90 % of cardiac patients who underwent provocation process with increasing doses of aspirin could tolerate upwardly to 1600 mg of the drug. If a rapid introduction of aspirin therapy is needed in a patient with cardiovascular illness and ASA-hypersensitivity, desensitization should be considered as the beginning choice.
In patients who accept contraindications to aspirin desensitization utilise of alternative handling is recommended [78] (Fig. 1).
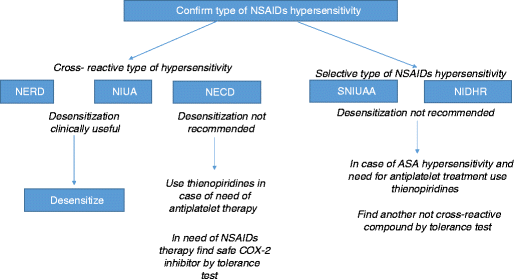
Steps in management in different subtypes of NSAIDs hypersensitivity. NERD (NSAIDS-exacerbated respiratory disease), NIUA (NSAIDs-induced urticaria/angioedema), NECD (NSAIDs-exacerbated cutaneous affliction), SNIUAA (single NSAIDs-induced urticaria/angioedema/anaphylaxis), NIDHR (NSAIDs-induced delayed hypersensitivity reaction).
Conclusions
Hypersensitivity to aspirin and other NSAIDs is quite common in the community. Aging population have greater needs to exist treated with aspirin or other NSAIDs to preclude cardiovascular events, cancers and to improve control of rhinosinusitis and asthma, thus may be at higher gamble for development of hypersensitivity reactions. Due to its infrequent pharmacological properties, aspirin is non easily replaceable in clinic and yet is a cheap drug. For some patients, desensitization to aspirin may be a toll-effective arroyo, although patients should be carefully selected for this procedure and the adventure-do good ratio of the process and chronic handling with aspirin should be taken into consideration.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted every bit: • Of importance •• Of major importance
-
Conaghan PG. A turbulent decade for NSAIDs: update on electric current concepts of nomenclature, epidemiology, comparative efficacy, and toxicity. Rheumatol Int. 2012;32:1491–502.
-
Kowalski ML, Makowska JS, Blanca M, et al. Hypersensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs)—classification, diagnosis and management: review of the EAACI/ENDA(#) and GA2LEN/HANNA*. Allergy. 2011;66:818–29.
-
Szczeklik A, Nizankowska E, Duplaga Thousand. Natural history of aspirin-induced asthma. AIANE Investigators European Network on Aspirin-Induced Asthma Eur Respir J. 2000;16:432–6.
-
Kowalski ML, Asero R, Bavbek S, et al. Classification and applied approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs. Allergy. 2013;68:1219–32. Position paper of EAACI on NSAIDs hypersensitivity, proposing new nomenclature of NSAIDs hypersensitivity and evidence-based approach to patients with dissimilar types of NSAIDs hypersensitivity.
-
Demoly P, Adkinson NF, Brockow K, et al. International Consensus on drug allergy. Allergy. 2014;69:420–37. International consensus on drug allergy, proposing diagnostic tools and management rules for drug hypersensitivity.
-
Samter M, Beers Jr RF. Intolerance to aspirin. Clinical studies and consideration of its pathogenesis. Ann Intern Med. 1968;68:975–83.
-
Kowalski ML, Cieslak K, Perez-Novo CA, Makowska JS, Bachert C. Clinical and immunological determinants of astringent/refractory asthma (SRA): association with Staphylococcal superantigen-specific IgE antibodies. Allergy. 2011;66:32–8.
-
Celik G, Pasaoglu 1000, Bavbek S, et al. Tolerability of selective cyclooxygenase inhibitor, celecoxib, in patients with analgesic intolerance. J Asthma. 2005;42:127–31.
-
Bavbek Southward, Celik G, Ozer F, Mungan D, Misirligil Z. Safety of selective COX-2 inhibitors in aspirin/nonsteroidal anti-inflammatory drug-intolerant patients: comparison of nimesulide, meloxicam, and rofecoxib. J Asthma. 2004;41:67–75.
-
Asero R. Adventure factors for acetaminophen and nimesulide intolerance in patients with NSAID-induced pare disorders. Ann Allergy Asthma Immunol. 1999;82:554–8.
-
Swierczynska-Krepa M, Sanak M, Bochenek G, Strek P, Cmiel A, Gielicz A, Plutecka H, Szczeklik A, Nizankowska-Mogilnicka E. Aspirin desensitization in patients with aspirin-induced and aspirin-tolerant asthma: A double-bullheaded study. J Allergy Clin Immunol 2014. Very of import placebo-controlled study proving efficacy of aspirin desensitization and aspirin treatment in patients with asthma, nasal polyposis and NSAIDs hypersensitivity.
-
Berges-Gimeno MP, Simon RA, Stevenson DD. Long-term treatment with aspirin desensitization in asthmatic patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2003;111:180–6.
-
Mastalerz L, Setkowicz M, Sanak Thousand, Szczeklik A. Hypersensitivity to aspirin: common eicosanoid alterations in urticaria and asthma. J Allergy Clin Immunol. 2004;113:771–5.
-
Dona I, Blanca-Lopez N, Jagemann LR, et al. Response to a selective COX-2 inhibitor in patients with urticaria/angioedema induced by nonsteroidal anti-inflammatory drugs. Allergy. 2011;66:1428–33.
-
Simon RA. Prevention and treatment of reactions to NSAIDs. Clin Rev Allergy Immunol. 2003;24:189–98.
-
Slowik SM, Slavin RG. Aspirin desensitization in a patient with aspirin sensitivity and chronic idiopathic urticaria. Ann Allergy Asthma Immunol. 2009;102:171–two.
-
Grzelewska-Rzymowska I, Roznlecki J, Szmidt Thou. Aspirin "desensitization" in patients with aspirin-induced urticaria and angioedema. Allergol Immunopathol (Madr). 1988;16:305–8.
-
Dona I, Blanca-Lopez N, Cornejo-Garcia JA, et al. Clin Exp Allergy. 2011;41:86–95. Study presenting accomplice of patients with cantankerous-reactive and single –reactive types of NSAIDs hypersensitivity.
-
Cortellini G, Testi S, Severino M, et al. Aspirin challenge/desensitisation before coronary stenting in subjects with history of hypersensitivity. A pragmatic arroyo. Eur Ann Allergy Clin Immunol. 2012;44:160–two. The study proposing approach to patients with need of antiplatelet handling based on stratification of reaction severity.
-
Wong JT, Nagy CS, Krinzman SJ, Maclean JA, Bloch KJ. Rapid oral claiming-desensitization for patients with aspirin-related urticaria-angioedema. J Allergy Clin Immunol. 2000;105:997–1001.
-
Silberman S, Neukirch-Stoop C, Steg PG. Rapid desensitization procedure for patients with aspirin hypersensitivity undergoing coronary stenting. Am J Cardiol. 2005;95:509–10.
-
Kowalski ML, Bienkiewicz B, Woszczek Grand, Iwaszkiewicz J, Poniatowska M. Diagnosis of pyrazolone drug sensitivity: clinical history versus peel testing and in vitro testing. Allergy Asthma Proc. 1999;20:347–52.
-
Pirmohamed M, James S, Meakin S, et al. Adverse drug reactions equally cause of admission to hospital: prospective analysis of 18 820 patients. BMJ. 2004;329:15–9.
-
Gebhardt M, Wollina U. Cutaneous side-effects of nonsteroidal anti-inflammatory drugs (NSAID). Z Rheumatol. 1995;54:405–12.
-
Patel MR, Marfatia YS. Clinical written report of cutaneous drug eruptions in 200 patients. Indian J Dermatol Venereol Leprol. 2008;74:430.
-
Barbaud A. Contact dermatitis due to topical drugs. M Ital Dermatol Venereol. 2009;144:527–36.
-
Ward KE, Archambault R, Mersfelder TL. Severe adverse peel reactions to nonsteroidal antiinflammatory drugs: a review of the literature. Am J Health Syst Pharm. 2010;67:206–13.
-
Mockenhaupt M, Kelly JP, Kaufman D, Stern RS. The hazard of Stevens-Johnson syndrome and toxic epidermal necrolysis associated with nonsteroidal antiinflammatory drugs: a multinational perspective. J Rheumatol. 2003;30:2234–40.
-
Sidoroff A, Dunant A, Viboud C, et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational instance–control study (EuroSCAR). Br J Dermatol. 2007;157:989–96.
-
Mihovilovic G, Ljubanovic D, Knotek Chiliad. Safe administration of celecoxib to a patient with repeated episodes of nephrotic syndrome induced past NSAIDs. Clin Drug Investig;31:351–v.
-
Ameen KH, Pinninti R, Jami S. Aceclofenac induced Stevens-Johnson/toxic epidermal necrolysis overlap syndrome. J Pharmacol Pharmacother. 2013;iv:69–71.
-
Rozieres A, Vocanson Chiliad, Said BB, Nosbaum A, Nicolas JF. Role of T cells in nonimmediate allergic drug reactions. Curr Opin Allergy Clin Immunol. 2009;9:305–10.
-
Pichler WJ. Delayed drug hypersensitivity reactions. Ann Intern Med. 2003;139:683–93.
-
Cernadas JR, Brockow G, Romano A, et al. General considerations on rapid desensitization for drug hypersensitivity—a consensus statement. Allergy. 2010;65:1357–66.
-
Halvorsen S, Andreotti F, x Berg JM, et al. Aspirin therapy in primary cardiovascular illness prevention: a position newspaper of the European Society of Cardiology working group on thrombosis. J Am Coll Cardiol. 2014;64:319–27.
-
Smith Jr SC, Allen J, Blair SN, et al. Aha/Acc, National Heart L, Blood I. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Eye, Lung, and Claret Found. Circulation. 2006;113:2363–72.
-
Ferrandez A, Piazuelo Due east, Castells A. Aspirin and the prevention of colorectal cancer. Best Pract Res Clin Gastroenterol. 2012;26:185–95.
-
Trabert B, Ness RB, Lo-Ciganic WH, et al. Aspirin, nonaspirin nonsteroidal anti-inflammatory drug, and acetaminophen use and risk of invasive epithelial ovarian cancer: a pooled assay in the Ovarian Cancer Association Consortium. J Natl Cancer Inst. 2014;106:djt431.
-
Nicholas G, Townsend North, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35:2950–9.
-
Bhatt DL. Can clopidogrel and aspirin lower mortality in patients with acute myocardial infarction? Nat Clin Pract Cardiovasc Med. 2006;3:182–iii.
-
Theroux P, Ouimet H, McCans J, et al. Aspirin, heparin, or both to care for acute unstable angina. North Engl J Med. 1988;319:1105–11.
-
Chen ZM, Sandercock P, Pan HC, et al. Indications for early aspirin use in astute ischemic stroke: a combined analysis of 40 000 randomized patients from the chinese acute stroke trial and the international stroke trial. On behalf of the CAST and IST collaborative groups. Stroke. 2000;31:1240–9.
-
Yusuf Due south, Zhao F, Mehta SR, Chrolavicius Due south, Tognoni G, Play a trick on KK. Clopidogrel in unstable angina to preclude recurrent events trial I. Effects of clopidogrel in improver to aspirin in patients with acute coronary syndromes without ST-segment tiptop. N Engl J Med. 2001;345:494–502.
-
Fox KA, Mehta SR, Peters R, et al. Clopidogrel in unstable angina to forbid recurrent ischemic events T. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent recurrent ischemic events (CURE) trial. Circulation. 2004;110:1202–8.
-
Anderson JL, Adams CD, Antman EM, et al. American College of C, American Heart Clan Task Force on Practice G, American College of Emergency P, Guild for Cardiovascular A, Interventions, Gild of Thoracic Southward, American Clan of C, Pulmonary R, Guild for Academic Emergency M. ACC/AHA 2007 guidelines for the management of patients with unstable angina/not-ST-Elevation myocardial infarction: a study of the American Higher of Cardiology/American Middle Association Task Force on Exercise Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Pinnacle Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Guild of Thoracic Surgeons endorsed past the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–e157.
-
Hamm CW, Bassand JP, Agewall S, et al. Guidelines ESCCfP. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of astute coronary syndromes (ACS) in patients presenting without persistent ST-segment superlative of the European Gild of Cardiology (ESC). Eur Heart J. 2011;32:2999–3054.
-
De Luca Grand, Verdoia Thou, Binda M, Schaffer A, Suryapranata H, Marino P. Aspirin desensitization in patients undergoing planned or urgent coronary stent implantation. A single-center experience. Int J Cardiol. 2013;167:561–two.
-
Comert Due south, Celebioglu E, Yucel T, et al. Aspirin 300 mg/twenty-four hours is effective for treating aspirin-exacerbated respiratory disease. Allergy. 2013;68:1443–51.
-
Berges-Gimeno MP, Simon RA, Stevenson DD. Early furnishings of aspirin desensitization treatment in asthmatic patients with aspirin-exacerbated respiratory affliction. Ann Allergy Asthma Immunol. 2003;90:338–41.
-
Sugariness JM, Stevenson DD, Simon RA, Mathison DA. Long-term effects of aspirin desensitization—treatment for aspirin-sensitive rhinosinusitis-asthma. J Allergy Clin Immunol. 1990;85:59–65.
-
Gosepath J, Schafer D, Mann WJ. Aspirin sensitivity: long term follow-upward afterwards upward to three years of adaptive desensitization using a maintenance dose of 100 mg of aspirin a day. Laryngorhinootologie. 2002;81:732–8.
-
Rozsasi A, Polzehl D, Deutschle T, et al. Long-term treatment with aspirin desensitization: a prospective clinical trial comparing 100 and 300 mg aspirin daily. Allergy. 2008;63:1228–34.
-
Kowalski ML, Grzelewska-Rzymowska I, Szmidt One thousand, Rozniecki J. Clinical efficacy of aspirin in "desensitised" aspirin-sensitive asthmatics. Eur J Respir Dis. 1986;69:219–25.
-
Stevenson DD. Diagnosis, prevention and treatment of adverse reactions to aspirin and nonsteroidal anti-inflammatory drugs. J Allergy Clin Immunol. 1984;74:617–22.
-
Cho KS, Soudry Eastward, Psaltis AJ, et al. Long-term sinonasal outcomes of aspirin desensitization in aspirin exacerbated respiratory disease. Otolaryngol Head Neck Surg. 2014;151:575–81.
-
Lee JY, Simon RA, Stevenson DD. Selection of aspirin dosages for aspirin desensitization handling in patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2007;119:157–64.
-
Woessner KM, White AA. Evidence-based approach to aspirin desensitization in aspirin-exacerbated respiratory illness. J Allergy Clin Immunol. 2014;133:286–7. e1-9.
-
Promise AP, Woessner KA, Simon RA, Stevenson DD. Rational approach to aspirin dosing during oral challenges and desensitization of patients with aspirin-exacerbated respiratory illness. J Allergy Clin Immunol. 2009;123:406–ten.
-
Macy East, Bernstein JA, Castells MC, et al. Aspirin challenge and desensitization for aspirin-exacerbated respiratory disease: a practice paper. Ann Allergy Asthma Immunol. 2007;98:172–4.
-
White AA, Stevenson DD, Simon RA. The blocking effect of essential controller medications during aspirin challenges in patients with aspirin-exacerbated respiratory disease. Ann Allergy Asthma Immunol. 2005;95:330–5.
-
Szmidt M, Grzelewska-Rzymowska I, Kowalski ML, Rozniecki J. Tolerance to acetylsalicylic acid (ASA) induced in ASA-sensitive asthmatics does not depend on initial adverse reaction. Allergy. 1987;42:182–5.
-
White AA, Bosso JV, Stevenson DD. The clinical dilemma of "silent desensitization" in aspirin-exacerbated respiratory illness. Allergy Asthma Proc. 2013;34:378–82.
-
Stevenson DD, Simon RA. Selection of patients for aspirin desensitization treatment. J Allergy Clin Immunol. 2006;118:801–four.
-
Knight A. Desensitization to aspirin in aspirin-sensitive patients with rhino-sinusitis and asthma: a review. J Otolaryngol. 1989;18:165–seven.
-
Dor PJ, Vervloet D, Baldocchi G, Charpin J. Aspirin intolerance and asthmal induction of a tolerance and long-term monitoring. Clin Allergy. 1985;xv:37–42.
-
Chiu JT. Improvement in aspirin-sensitive asthmatic subjects after rapid aspirin desensitization and aspirin maintenance (ADAM) handling. J Allergy Clin Immunol. 1983;71:560–seven.
-
Naeije N, Bracamonte M, Michel O, Sergysels R, Duchateau J. Furnishings of chronic aspirin ingestion in aspirin-intolerant asthmatic patients. Ann Allergy. 1984;53:262–4.
-
Kowalski ML, Grzelewska-Rzymowska I, Rozniecki J, Szmidt Thou. Aspirin tolerance induced in aspirin-sensitive asthmatics. Allergy. 1984;39:171–8.
-
Wallace JL, Syer S, Denou E, et al. Proton pump inhibitors exacerbate NSAID-induced small abdominal injury by inducing dysbiosis. Gastroenterology. 2011;141:1314–22. 22 e1-5.
-
Marlicz W, Loniewski I, Grimes DS, Quigley EM. Nonsteroidal anti-inflammatory drugs, proton pump inhibitors, and gastrointestinal injury: contrasting interactions in the stomach and modest intestine. Mayo Clin Proc. 2014;89:1699–709.
-
Scheiman JM. The use of proton pump inhibitors in treating and preventing NSAID-induced mucosal damage. Arthritis Res Ther. 2013;15 Suppl 3:S5.
-
McMullan KL, Wedner HJ. Prophylactic of aspirin desensitization in patients with reported aspirin allergy and cardiovascular affliction. Clin Cardiol. 2013;36:25–30.
-
Fajt ML, Petrov AA. Outpatient aspirin desensitization for patients with aspirin hypersensitivity and cardiac affliction. Crit Pathw Cardiol. 2011;ten:17–21.
-
Alijotas-Reig J, San Miguel-Moncin K, Cistero-Bahima A. Aspirin desensitization in the handling of antiphospholipid syndrome during pregnancy in ASA-sensitive patients. Am J Reprod Immunol. 2006;55:45–50.
-
Dalmau Yard, Gaig P, Gazquez Five, Merce J. Rapid desensitization to acetylsalicylic acid in acute coronary syndrome patients with NSAID intolerance. Rev Esp Cardiol. 2009;62:224–5.
-
Rossini R, Angiolillo DJ, Musumeci G, et al. Aspirin desensitization in patients undergoing percutaneous coronary interventions with stent implantation. Am J Cardiol. 2008;101:786–ix.
-
Ortega-Loayza AG, Raza Southward, Minisi AJ, Topaz O, Heller A, Jovin IS. Aspirin desensitization/claiming in three patients with unstable angina. Am J Med Sci. 2010;340:418–xx.
-
Pattanaik D, Lieberman P, Das P. Aspirin sensitivity and coronary artery disease: implications for the practicing cardiologist. Hereafter Cardiol. 2012;8:555–62.
Source: https://link.springer.com/article/10.1007/s40521-015-0049-x

0 Response to "How To Desensitize The Tip Domain_10"
Post a Comment